Etiological Evaluation of Microcytic Hypochromic Anemia at a Tertiary Care Hospital in the Eastern Part of India
Abstract
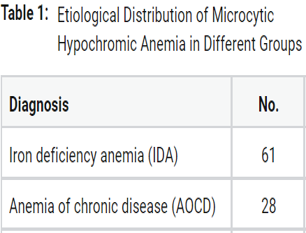
Microcytic hypochromic anemia is a part anemia classification based on the morphology of anemia with well-known causes and management. The causes of microcytic hypochromic anemia may be either due to iron deficiency anemia, anemia of inflammation, or thalassemia. There are lots of recent advancements and studies done on the etiology of Microcytic Hypochromic anemia but accurate data especially from the eastern part of India are notavailable. To investigate the causes of Microcytic Hypochromic anaemia at a tertiary care centre in eastern India. After obtaining valid written consent, cases of microcytic hypochromic anaemia were selected from the OPD and indoors for this cross-sectional investigation. The whole haematological and biochemical investigations were sent for anaemia workup. The study comprised 100 patients with microcytic hypochromic disorder. The study comprised subjects ranging in age from 18 to 80 years. 39% were men and 61% were women. In thalassemia patients, the most common were b-thalassemia traits in 81.8 %, followed by 9% of each Delta B–thalassemia and double heterozygous HBE and beta thalassemia. Anemia is not an illness in and of itself, but rather a symptom of another, hence finding the underlying cause is significantly more important. The diagnosis of microcytic hypochromic anaemia is insufficient in the absence of an underlying cause. Special precautions will be made to determine the cause of iron deficient anaemia. The thalassemia trait must also be diagnosed in order to minimise excessive iron supplementation and for family screening.
Full text article
References
C M Chaparro and P S Suchdev. Anemia epidemiology, pathophysiology, and etiology in low- and middle- income countries. Annals of the new York Academy of Sciences, 1450(1):15– 31, 2019.
P Dasharatham and V S Reddy. A study of etiological and clinical profile of patients with severe anemia in a tertiary care hospital. Int J Adv Med, 5:1422–1429, 2018.
Ministry of Health and Family Welfare. National Family Health Survey (NFHS 5) 2019-2021, 2022. Government of India.
P R Dallman. Diagnosis of anemia and iron deficiency: analytic and biological variations of laboratory tests. The American journal of clinical nutrition, 39(6):937–941, 1984.
M Wiciński, G Liczner, K Cadelski, T Kołnierzak, M Nowaczewska, and B Malinowski. Anemia of Chronic Diseases: Wider Diagnostics-Better Treatment? Nutrients, 12(6):1784, 2020.
W O Uprichard and J Uprichard. Investigating microcytic anaemia. Bmj, 346:3154, 2013.
J F Matos, L Dusse, K B Borges, R L De Castro, W Coura-Vital, and M D G Carvalho. A new index to discriminate between iron deficiency anemia and thalassemia trait. Revista brasileira de hematologia e hemoterapia, 38:214–219, 2016.
S Majid, M Salih, R Wasaya, and W Jafri. Predictors of gastrointestinal lesions on endoscopy in iron deficiency anemia without gastrointestinal symptoms. BMC gastroenterology, 8(1):1– 7, 2008.
A Zhu, M Kaneshiro, and J D Kaunitz. Evaluation and treatment of iron deficiency anemia: a gastroenterological perspective. Digestive diseases and sciences, 55(3):548–559, 2010.
M Alleyne, M K Horne, and J L Miller. Individualized treatment for iron-deficiency anemia in adults. The American journal of medicine, 121(11):943–948, 2008.
S Patel, M Shah, J Patel, and N Kumar. Iron deficiency anaemia in moderate to severe anaemic patients. Gujarat Medical Journal, 64, 2009.
L Raman, M K Menon, and P K Devi. Anaemia in pregnancy. Postgraduate obstetrics and gynaecology. volume 128 of 1, pages 45–51, 1986. 3rd edition: p 55-62. Hyderabad: Orient Longmans. 008 Jul.
S F Clark. Iron deficiency anemia. Nutrition in clinical practice, 23(2):128–141, 2008.
M T Kepczyk and C S C Kadakia. Prospective evaluation of gastrointestinal tract in patients with iron-deficiency anemia. Digestive diseases and sciences, 40(6):1283–1289, 1995.
S Serefhanoglu, Y Buyukasik, H Emmungil, N Sayinalp, I C Haznedaroglu, H Goker, and O I Ozcebe. Identification of clinical and simple laboratory variables predicting responsible gastrointestinal lesions in patients with iron deficiency anemia. International journal of medical sciences, 8(1):30, 2011.
D C Rockey. Occult gastrointestinal bleeding. New England Journal of Medicine, 341(1):38–46, 1999.
A Jacobs and E B Butler. Menstrual blood-loss in iron-deficiency anaemia. Lancet, 2:407–409, 1965.
J B Sharma, B S Arora, and S Kumar. Helminth and protozoan intestinal infections: An important cause for anemia in pregnant women in Delhi. J ObstetGynaecol Ind, 51(6):58–61, 2000.
E A Price and S L Schrier. Unexplained aspects of anemia of inflammation. Advances in hematology, 2010.
G Weiss. Pathogenesis and treatment of anaemia of chronic disease. Blood reviews, 16(2):87–96, 2002.
E Joosten and P Lioen. Iron deficiency anemia and anemia of chronic disease in geriatric hospitalized patients: How frequent are comorbidities as an additional explanation for the anemia? Geriatrics and gerontology international, 15(8):931–935, 2015.
B J Mccranor, J M Langdon, O D Prince, L K Femnou, A E Berger, C Cheadle, and C N Roy. Investigation of the role of interleukin-6 and hepcidin antimicrobial peptide in the development of anemia with age. Haematologica, 98(10):1633–1640, 2013.
P Papathakis and E Piwoz. Nutrition and Tuberculosis: A review of the literature and considerations for TB control programs. United States Agency for International Development, Africa’s Health 2010 Project, 1, 2008.
M Van Lettow, C E West, J W M Van Der Meer, F T Wieringa, and R D Semba. Low plasma selenium concentrations, high plasma human immunodeficiency virus load and high interleukin-6 concentrations are risk factors associated with anemia in adults presenting with pulmonary tuberculosis in Zomba district. European journal of clinical nutrition, 59(4):526–532, 2005.
Sunanda Mondal et al. A Study on Microcytic Hypochromic Anaemia with the Help of Parameters: CBC with RBC Indices, Biochemical Markers (Iron Profile) and HPLC - A Hospital Based Observational Study. JMSCR, 05(07):24986–24992, 2017.
D R Higgs, S L Thein, and W G Wood. Distribution and population genetics of the thalassemias. 2001. In: Weatherall DJ, Clegg JB, editors. The Thalassemia Syndromes. 4th ed. Oxford: Blackwell Science, pp. 237–84. ISBN: 978-0-470-69594-4.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.