Abstract
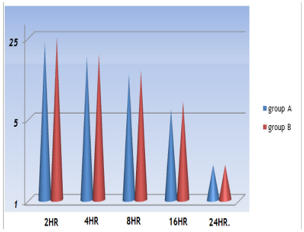
One of the most common procedures in our days is the laparoscopic cholecystectomy, is regarded as the best option for the management of gallstones, but the matter of using subhepatic drain or not using it; remain a matter of debate between surgeons. The aim of this study is to evaluate the role of drain in uncomplicated cases of laparoscopic cholecystectomy and its effect in the minimizing the postoperative morbidity. One hundred patients were undergoing laparoscopic cholecystectomy in the Diwania Teaching Hospital chosen randomly from the period 1st of October 2014 to the 30 January 2017, fifty patients from them named as group A and they underwent uncomplicated Laparoscopic cholecystectomy with a drain in the right sub hepatic region and the other group which is group B they also underwent uncomplicated laparoscopic cholecystectomy but with no drain, a Comparison between the two groups take place to detect the incidence of nausea, vomiting, postoperative pain, hospital stay and the morbidity in these two groups by using a visual analog scale. Nausea and vomiting in the two groups show no considerable differences at the various periods postoperatively; while the hospital stays showing significant differences as well as the postoperative abdominal and shoulder tip pain in the group with drain more than the group without drain. The resignation of using drains in the cases of uncomplicated laparoscopic cholecystectomy minimizing the post-operative complication and morbidity.
Full text article
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.