Abstract
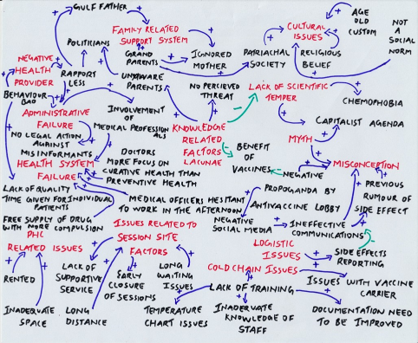
Vaccinations are given to healthy people to prevent specific diseases which are proven tool of public health. Nowadays lot of hesitant movement are active around the globe. Application of system thinking should be adopted to solve this complex phenomenon. The objective is to study the barriers and solutions of Immunization enlisted by Policy makers and administrators at Malappuram district, Kerala, South India. Descriptive qualitative method was the design espoused in this study. Free listing is the technique adopted to enlist barriers and solution at Malappuram district. The data was analysed using Visual Anthropac software. Further barriers and solutions of immunization was enumerated on basis of descending order of Smith S value. Causal loop diagram was used to depict complex phenomenon regarding barriers of immunization. The policy makers and administrators had solicited barriers as Religious belief, antivaccine lobby, negative propaganda by alternative systems and ineffective logistic management. The main solutions set forth to break barriers were strengthening Information Education Communication (IEC), bring in behavioural change communication and adopt policy reforms. The study determined by conscripting community and health system enabled barriers, with solutions for it encompassing global networking, engaging various stake holders and applying system approach for health system strengthening.
Full text article
References
Adam, T., de Savigny, D. 2012. Systems thinking for strengthening health systems in LMICs: need for a paradigm shift. Health Policy and Planning, 27(suppl 4):iv1–iv3.
Centola, D., Macy, M. 2007. Complex Contagions and the Weakness of Long Ties. American Journal of Sociology, 113(3):702–734.
Dubé, E., Laberge, C., Guay, M., Bramadat, P., Roy, R., Bettinger, J. A. 2013. Vaccine hesitancy: an overview. Human Vaccines & Immunotherapeutics, 9(8):1763–1773.
Dushoff, J., Plotkin, J. B., Viboud, C., Simonsen, L., Miller, M., Loeb, M., Earn, D. J. D. 2007. Vaccinating to Protect a Vulnerable Subpopulation. PLoS Medicine, 4(5):e174.
Hunter, D. J., Rayner, G. 2004. The UK Public Health Association and Congress of the World Federation of Public Health Associations (WFPHA) conference—plenary session presentations. Public Health, 118(7):461–487.
Kadri, A. M., Singh, A., Jain, S., Mahajan, R. G., Trivedi, A. 2010. Study on immunization coverage in urban slums of Ahmedabad city. Health and population: Perspectives and Issues, 33(1):50–54.
Kumru, O. S., Joshi, S. B., Smith, D. E., Middaugh, C. R., Prusik, T., Volkin, D. B. 2014. Vaccine instability in the cold chain: Mechanisms, analysis and formulation strategies. Biologicals, 42(5):237–259.
Okonko, I. O., Nkang, A. O., Udeze, A. O., Adedeji, A. O., Ejembi, J., Onoja, B. A., Garba, K. N. 2013. Global eradication of measles: A highly contagious and vaccine preventable disease-what went wrong in Africa? Journal of Cell and Animal Biology, 3(8):119–140.
Peters, D. H. 2014. The application of systems thinking in health: why use systems thinking? Health Research Policy and Systems, 12(1):1–6.
Salgado, C. D., Giannetta, E. T., Hayden, F. G., Farr, B. M. 2004. Preventing Nosocomial Influenza by Improving the Vaccine Acceptance Rate of Clinicians. Infection Control & Hospital Epidemiology, 25(11):923–928.
Sterman, J. D. 2006. Learning from Evidence in a Complex World. American Journal of Public Health, 96(3):505–514.
Tafuri, S., Gallone, M. S., Cappelli, M. G., Martinelli, D., Prato, R., Germinario, C. 2014. Addressing the anti-vaccination movement and the role of HCWs. Vaccine, 32(38):4860–4865.
Techathawat, S., Varinsathien, P., Rasdjarmrearnsook, A., Tharmaphornpilas, P. 2007. Exposure to heat and freezing in the vaccine cold chain in Thailand. Vaccine, 25(7):1328–1333.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.