Abstract
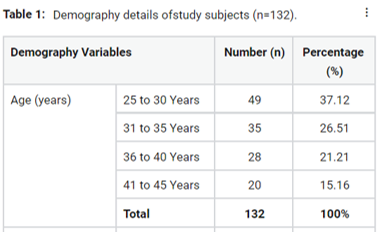
Even till now, nothing much has been done to explore the inflammation and prevention of the same around the implants placed, hence the aim of this study was to evaluate factor associated with dentist knowledge, attitude along with practice in preventing peri-implant diseases. This was a descriptive, cross-sectional, questionnaire based study carried within Dental professionals of Patna city. Stratified random sampling technique was the sampling method utilized in this study. The survey was conducted among 132 dentists. A questionnaire was framed by using google forms. Most of dental professionals were having fair knowledge {61(46.21%)}, positive attitude {61 (46.21%)} and poor practice (47.72%)} towards prevention of Peri-implant diseases. On application of Chi-square test, it was found that knowledge of study participants was significantly (0.05*) associated with gender, average duration of doing Implant surgery while attitude was significantly (0.05*) associated with age and degree. It was concluded that knowledge was fair; attitude was positive and despite this practice was poor regarding the prevention of Peri-Implant diseases among Dental professionals. Factors associated with knowledge, attitude and practice of study participants was gender, average duration of doing Implant surgery, age and degree.
Full text article
References
Arora, A., Datarkar, A. N., Borle, R. M., Rai, A., Adwani, D. G. 2013. Custom-Made Implant for Maxillofacial Defects Using Rapid Prototype Models. Journal of Oral and Maxillofacial Surgery, 71(2):e104–e110.
Berglundh, T., Persson, L., Klinge, B. 2002. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. Journal of Clinical Periodontology, 29(3):197–212.
Blanes, R. J., Bernard, J. P., Blanes, Z. M., Belser, U. C. 2007. A 10-year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clinical Oral Implants Research, 18(6):707– 714.
Donos, N., Mardas, N., Buser, D. 2009. An outline of competencies and the appropriate postgraduate educational pathways in implant dentistry. European Journal of Dental Education, 13:44–54.
Doornewaard, R., Jacquet, W., Cosyn, J., De Bruyn, H. 2018. How do peri-implant biologic parameters correspond with implant survival and periimplantitis? A critical review. Clinical Oral Implants Research, 29 Suppl 1:100–123.
Jemt, T., Olsson, M., Renouard, F., Stenport, V., Friberg, B. 2016. Early Implant Failures Related to Individual Surgeons: An Analysis Covering 11,074 Operations Performed during 28 Years. Clinical Implant Dentistry and Related Research, 18(5):861–872.
Ji, T.-J., Kan, J. Y. K., Rungcharassaeng, K., Roe, P., Lozada, J. L. 2012. Immediate Loading of Maxillary and Mandibular Implant-Supported Fixed Complete Dentures: A 1- to 10-Year Retrospective Study. Journal of Oral Implantology, 38(S1):469– 477.
Kadkhodazadeh, M., Hosseinpour, S., Kermani, M. E., Amid, R. 2018. Knowledge and Attitude of Iranian Dentists towards Peri-implant Diseases. Journal of Periodontology & Implant Dentistry, 9(1):12–17.
Lambert, P. M., Morris, H. F., Ochi, S. 1997. Positive Effect of Surgical Experience With Implants on Second-Stage Implant Survival. Journal of Oral and Maxillofacial Surgery, 55(12):12–18.
Lindhe, J., Meyle, J. 2008. Peri-implant diseases: Consensus Report of the Sixth European Work shop on Periodontology. Journal of Clinical Periodontology, 35(8):282–285.
Meher, A. H., Shrivastav, S. S., Vibhute, P. J., Hazarey, P. V. 2012. Deflection and stress distribution around mini-screw implants: A finite element investigation into the effect of cortical bone thickness, force magnitude and direction. Journal of Orthodontics, 39(4):249–255.
Morris, H. F., Manz, M. C., Tarolli, J. H. 1997. Success of Multiple Endosseous Dental Implant Designs to Second-Stage Surgery Across Study Sites. Journal of Oral and Maxillofacial Surgery, 55(12):76–82.
Renvert, S., Persson, G. R., Pirih, F. Q., Camargo, P. M. 2018. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations. Journal of Clinical Periodontology, 45:S278–S285.
Shilpa, B. S., Vasudevan, S. D., Bhongade, M. L., Baliga, V., Pakhare, V. V., Dhadse, P. V. 2018. Evaluation of survival of 8 mm-length implants in posterior resorbed ridges: A pilot study. Journal of Indian Society of Periodontology, 22(4):334–334.
Tolstunov, L. 2007. Implant Zones of the Jaws: Implant Location and Related Success Rate. Journal of Oral Implantology, 33(4):211–220.
Tonetti, M. S., Chapple, I. L. C., Jepsen, S., Sanz, M. 2015. Primary and secondary prevention of periodontal and peri-implant diseases: Introduction to, and objectives of the 11th European Workshop on Periodontology consensus conference. Journal of Clinical Periodontology, 42:S1–S4.
Zitzmann, N. U., Berglundh, T. 2008. Definition and prevalence of peri-implant diseases. Journal of Clinical Periodontology, 35:286–291.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.