Drug Utilization Review of Antibiotics in Chronic Kidney Disease Patients and Comparison with the Standard Drug of Choice
Abstract
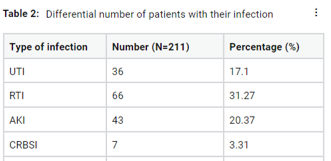
The risk of morbidity and death in patients with chronic kidney disease (CKD), formerly known as chronic renal failure (CRF), is increased by a number of comorbidities, including infections, cardiovascular disease (CVD), and anaemia. The second most common reason for death in this population is infections. Antibiotics can accumulate in the body and have harmful consequences when given to CKD patients without the necessary dosage modification and in an illogical manner. The purpose of this particular study was to compare the standard treatment protocol with the reasoning and prescribing patterns of antibiotics administered for infections in CKD patients staged 3-5 in the nephrology department of a single Center in Kerala’s Kottayam district. The medical records of 272 patients who met the inclusion and exclusion criteria and were admitted to the nephrology department between November 2019 and November 2020 were examined as part of single-centred retrospective research that was created to address this. Surprisingly, just 45 percent of the prescriptions were rational, while 55 percent of them were nonsensical. Additionally, we discovered that 23 percent of antibiotic selections went outside accepted therapeutic standards. Thus, we could conclude that the prescriber must use the utmost caution while prescribing to a patient with CKD to prevent future difficulties.
Full text article
References
A S Levey, K. U Eckardt, Y Tsukamoto, A Levin, J Coresh, J Rossert, D D E Zeeuw, T H Hostetter, N Lameire, and G Eknoyan. Definition and classification of chronic kidney disease: A position statement from kidney disease: Improving Global Outcomes (KDIGO). Kidney International, 67(6):2089–2100, 2005.
A C Webster, E V Nagler, R L Morton, and P Masson. Chronic kidney disease. Lancet, 389(16):32064–32069, 2017.
E Paul, Adeera Stevens, and Levin. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med, 158(11):825–855, 2013.
J Ishigami and K Matsushita. Clinical epidemiology of infectious disease among patients with chronic kidney disease. Clinical and Experimental Nephrology, 23(4):437–447, 2019.
Y Xie, B Bowe, A H Mokdad, H Xian, Y Yan, T Li, G Maddukuri, C. Y Tsai, T Floyd, and Z Al-Aly. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney International, 94(3):567–581, 2018.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.