Efficacy of Single Dose Oral Gabapentin in Day Care Laparoscopic Surgeries - A Randomized Double-blinded Placebo Control Study
Abstract
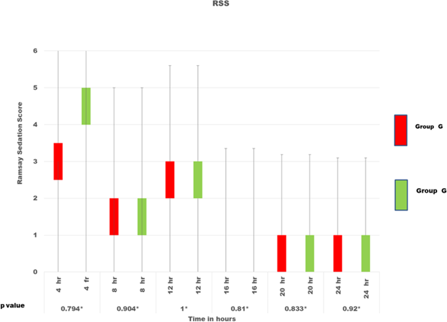
Gabapentin, an anticonvulsant, reduces postoperative pain and has an anti-emetic property by diminishing central sensitisation. We studied the effect of oral gabapentin on the recovery profile of daycare laparoscopic surgeries. One hundred patients undergoing daycare laparoscopic surgeries were randomly divided into two groups: Group G - Gabapentin 300mg and Group P - Placebo tablet was given orally one hour before surgery. General anaesthesia was standardized in both groups. The time taken to achieve a Modified Aldrete score of nine and duration of postoperative analgesia was observed. The Visual analogue score(VAS), hemodynamics, additional intraoperative fentanyl consumption and complications were also recorded. If VAS ≥ 3, Paracetamol 1g and if VAS ≥ 6, Tramadol 100mg was used. The total consumption of analgesics was noted. The continuous and categorical variables were assessed by unpaired student t-test and chi-square test, respectively. Both groups were demographically similar. The recovery time in the gabapentin group (5.18 ± 1.53 min) was similar to the control group (5.05 ± 1.62 min). The duration of analgesia was significantly prolonged in gabapentin (297.4 ± 120.86 min) than in the control (148.63 ± 48.92) group. The hemodynamics was significantly reduced during the first hour in the gabapentin group than in the control group. The additional fentanyl requirements, PONV were also significantly reduced in gabapentin while an increased incidence of dry mouth was observed. The use of a single dose of oral gabapentin in laparoscopic surgeries significantly prolonged the duration of postoperative analgesia with similar recovery time, reduced intraoperative fentanyl consumption, better hemodynamic stability and fewer complications.
Full text article
References
P Hayden and S Cowman. Anaesthesia for laparoscopic surgery. Continuing Education in Anaesthesia Critical Care & Pain, 11(5):177– 180, 2011.
F Gerges, G Kanazi, and S Jabbour-Khoury. Anesthesia for laparoscopy: a review. Journal of Clinical Anesthesia, 18(1):67–78, 2006.
K Kaur, P Arora, and S Singhal. Oral clonidine versus gabapentin as premedicant for obtunding hemodynamic response to laryngoscopy and tracheal intubation. Saudi Journal of Anaesthesia, 8(2):172–177, 2014.
Sara Mohamed, Abdel Naby, Alshaimaa Abdel Fattah Kamel, Amany Abdelghany, and Dina Abdelhameed Elsadek Salem. The Effects of Pre-emptive Single-Dose Oral Pregabalin on Maternal Anxiety and Stress Response to Laryngoscopic intubation During Caesarean Section. Egyptian Journal of Anaesthesia, 37(1):214–220, 2021.
B A Chizh, M Gohring, and A Troster. Effects of oral pregabalin and aprepitant on pain and central sensitization in the electrical hyperalgesia model in human volunteers. Br J Anaesth, 98(2):246–254, 2007.
A T Beck, C H Ward, M Mendelson, J Mock, and J Erbaugh. An inventory for measuring depression. Arch Gen Psychiatry, 4:561–571, 1961.
J Hah, S C Mackey, and P Schmidt. Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort: A Randomized Clinical Trial. JAMA Surg, 153(4):303–311, 2018.
Michael Verret, François Lauzier, Ryan Zarychanski, et al. Perioperative Use of Gabapentinoids for the Management of Postoperative Acute Pain: A Systematic Review and Meta-analysis. Anesthesiology, 133:265–279, 2020.
B Liu, R Liu, and L Wang. A meta-analysis of the preoperative use of gabapentinoids for the treatment of acute postoperative pain following spinal surgery. Medicine (Baltimore), 96(37):8031–8031, 2017.
C Chiu, P Aleshi, L J Esserman, C Inglis-Arkell, E Yap, E L Whitlock, and M W Harbell. Improved analgesia and reduced postoperative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy. BMC Anesthesiol, 18(1):41–41, 2018.
C K Pandey, S Priye, S Singh, U Singh, R B Singh, and P K Singh. Preemptive use of gabapentin significantly decreases postoperative pain and rescue analgesic requirements in laparoscopic cholecystectomy. Can J Anaesth, 51(4):358–63, 2004.
N T Siddiqui, A Yousefzadeh, M Yousuf, D Kumar, F K Choudhry, and Z Friedman. The Effect of Gabapentin on Delayed Discharge from the Postanesthesia Care Unit: A Retrospective Analysis. Pain Pract, 18(1):18–22, 2018.
L Wang, Y Dong, J Zhang, and H Tan. The efficacy of gabapentin in reducing pain intensity and postoperative nausea and vomiting following laparoscopic cholecystectomy: A meta analysis. Medicine, 96(37):8007–8017, 2017.
S Arumugam, C S Lau, and R S Chamberlain. Use of preoperative gabapentin significantly reduces postoperative opioid consumption: a meta-analysis. J Pain Res, 9:631–640, 2016.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.