Abstract
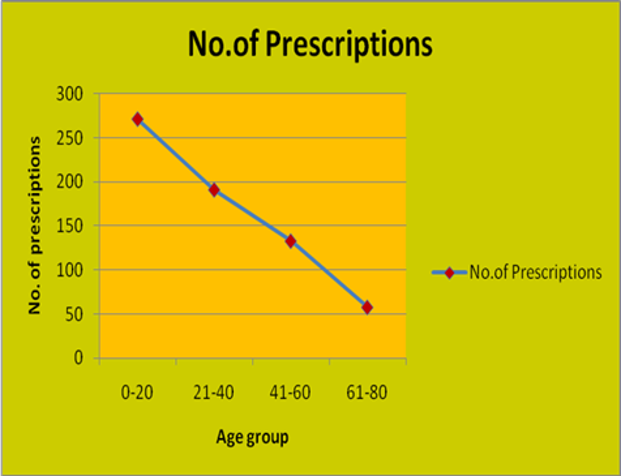
Pharmacoepidemiology deals with the use and effects of medications in a large number of population—the combination of epidemiology principles to the effects of drug and its usage. Pharmacoepidemiology helps in optimal utilization of medicines and assist health care providers in making better decisions on drug therapy that will tend to curtail the Drug-Drug interactions, thereby prevents alteration in the pharmacological activity of one drug by another. Among all types of interaction, Drug-Drug interaction causes a higher rate of mortality. A prospective study conducted with 653 prescriptions that were collected from the various regions of Andhra Pradesh like Kadapa, Proddatur, Pulivendula, Kurnool are checked in interaction checker, results are projected in 4 categories a) Age and Sex preponderance(Demographics) rate of drugs interaction b) Interaction rate of major/minor type c) Department wise - General medicine (72.37%), Gynaec (69.02%), Pediatric (29.33%), Ophthalmology (75%) d) Most common interacting pairs of various department Ex: Ceftriaxone & Furosemide, Diclofenac & Furosemide, Albuterol & Losartan are observed in General Medicine. Statistical significance (P-value 0.00002) is obtained based on One Way ANOVA. This study elucidates the significance of pharmacoepidemiology; however, this requires much efforts to prevent causation effects of drugs. It is helpful to locate them by the establishment of “Drug interaction monitoring program” or by establishing “Pharmacoepidemiological centres” in every hospital for the screening of prescriptions by “Pharmacist” and thereby edify doctors and public for better medication use.
Full text article
References
Armitage, P., Colton, T. 2005. Encyclopedia of Biostatistics. Wiley. Volume 8, Second Edition, ISBN: 978-0470849071.
Ballard, D., Bryant, S. C., Brien, D. 1994. Referral selection bias in the Medicare hospital mortality prediction model: are centers of referral for Medicare beneficiaries necessarily centers of excellence? Health Services Research, 28(6):771– 784.
Corder, G. W., Foreman, D. I. 2009. Nonparametric Statistics for Non-Statisticians: A Step-by-Step Approach. Wiley. First Edition, ISBN: 978- 0470454619, Pages 264.
Crane, J., Pearce, N., Burgess, C., Beasley, R. 1995. Asthma and the beta agonist debate. Thorax, 50(Suppl 1):S5–S10.
Halvorsen, K. H., Ruths, S., Granas, A. G., Viktil, K. K. 2010. Multidisciplinary intervention to identify and resolve drug-related problems in Norwegian nursing homes. Scandinavian Journal of Primary Health Care, 28(2):82–88.
Hennekens, C. H., Buring, J. E., Manson, J. E., Stampfer, M., Rosner, B., Cook, N. R., Belanger, C., LaMotte, F., Gaziano, J. M., Ridker, P. M., Willett, W., Peto, R. 1996. Lack of Effect of Long-Term Supplementation with Beta Carotene on the Incidence of Malignant Neoplasms and Cardiovascular Disease. New England Journal of Medicine, 334(18):1145– 1149.
Lau, D. T., Kasper, J. D., Potter, D. E. B., Lyles, A., Bennett, R. G. 2005. Hospitalization and Death Associated With Potentially Inappropriate Medication Prescriptions Among Elderly Nursing Home Residents. Archives of Internal Medicine, 165(1):68–74.
Maklan, C. W., Greene, R., Cummings, M. A. 1994. Methodological Challenges and Innovations in Patient Outcomes Research. Medical Care, 32(Suppl 7):JS13–JS21.
Melton, L. J. 1985. Selection Bias in the Referral of Patients and the Natural History of Surgical Conditions. Mayo Clinic Proceedings, 60(12):880–885.
Parthasarathi, G., Nyfort-Hansen, K., Nahata, M. C. 2012. A Textbook of Clinical Pharmacy Practice. Himayatnagar, Hyderabad. Universities Press. Chapter 24, ISBN: 9788173717567, page 408.
Porta, M. S., Hartzema, A. G. 1991. The contribution of epidemiology to the study of drugs. In Pharmacoepidemiology: An Introduction, Ohio. Harvey Whitney Books. Second Edition, Pages 2-17.
Primejdie, D. P., Mallet, L., Popa, A., Bojita, M. T. 2014. Description of a systematic pharmaceutical care approach intended to increase the appropriateness of medication use by elderly patients. Medicine and Pharmacy Reports, 87(2):119–129.
Sackett, D. L. 1979. Bias in analytic research. Journal of Chronic Diseases, 32(1-2):51–63.
Steineck, G., Ahlbom, A. 1992. A Definition of Bias Founded on the Concept of the Study Base. Epidemiology, 3(6):477–482.
Stockley, I. H. 2002. Stockley’s drug interactions. London, Chicago. Pharmaceutical Press. Sixth Edition, ISBN: 978-0853695042, Pages 960.
Strom, B. L. 1994. What is Pharmacoepidemiology? In Pharmacoepidemiology, New York. Wiley. Second Edition, Chapter 1, ISBN: 9780471940586, Pages 3-13.
Taylor, J. 1982. An Introduction to Error Analysis. Sausalito, California. University Science Books. Second Edition, ISBN: 0935702423. Pages 327.
Vonbach, P. 2007. Drug-Drug Interactions in the Hospital. Inaugural dissertation, University of Basel, zürich.
Wacholder, S., McLaughlin, J. K., Silverman, D. T., Mandel, J. S. 1992. Selection of Controls in Case-Control Studies. American Journal of Epidemiology, 135(9):1019–1028.
Wettermark, B. 2013. The intriguing future of pharmacoepidemiology. European Journal of Clinical Pharmacology, 69(S1):43–51.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.