Abstract
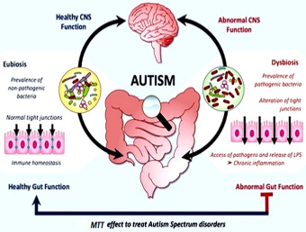
Autism spectrum disorder (ASD) is a developmental disorder that affects behaviour and communication. It can be diagnosed at any age, although the symptoms generally appear in the first two years of life. Autism is also known as a "spectrum" disorder because there is wide variation in the severity and type of patient experience. Intestinal dysbiosis remains a risk factor for several neuron-developmental disorders and physiological diseases such as ASD. The gut microbiome in human influence the total metabolomic profile and thus has an impact on the overall health of human. The brain-intestinal axis concept demonstrates the interaction between the brain and the diverse gut microbial population. Recent findings show that ASD symptoms in affected individuals are linked with the altered intestinal microbiome. The current treatment modality for the symptoms of ASD are limited to Applied Behaviour Analysis (ABA) and FDA approved medications like Risperidone and Aripiprazole. Individuals with ASD appear to be susceptible to adverse effects of these medications. Current accumulating studies indicate that Microbiota Transfer Therapy (MTT) is a promising technique for treating ASD. MTT involves in vitro batch culture of gut microbiota, which is viewed as a quick and accessible method. It has provided encouraging results by improving ASD-related gastrointestinal (GI) and behavioural symptoms in affected individuals. The present review focuses on the link between gut dysbiosis and ASD, analyses the available clinical studies related to various treatment options and describes the role of MTT as a promising therapy of bringing back the healthy gut microbiota composition in treating ASD.
Full text article
References
Abdellatif, B., McVeigh, C., Bendriss, G., Chaari, A. 2020. The Promising Role of Probiotics in Managing the Altered Gut in Autism Spectrum Disorders. International Journal of Molecular Sciences, 21(11):4159.
Adams, J. B., Baral, M., Geis, E., Mitchell, J., Ingram, J., Hensley, A., Zappia, I., Newmark, S., Gehn, E., Rubin, R. A., Mitchell, K., Bradstreet, J., El-Dahr, J. 2009. Safety and efficacy of oral DMSA therapy for children with autism spectrum disorders: Part A - Medical results. BMC Clinical Pharmacology, 9(1):16.
Andriamihaja, M., Lan, A., Beaumont, M., Audebert, M., Wong, X., Yamada, K., Yin, Y., Tomé, D., Carrasco-Pozo, C., Gotteland, M., Kong, X., Blachier, F. 2015. The deleterious metabolic and genotoxic effects of the bacterial metabolite p-cresol on colonic epithelial cells. Free Radical Biology and Medicine, 85:219–227.
Backhed, F. 2005. Host-Bacterial Mutualism in the Human Intestine. Science, 307(5717):1915–1920.
Bäckhed, F., Roswall, J., Peng, Y., Feng, Q., Jia, H., Kovatcheva-Datchary, P., Li, Y., Xia, Y., Xie, H., Zhong, H., Khan, M. T., Zhang, J., Li, J., Xiao, L., Al-Aama, J., Zhang, D., Lee, Y. S., Kotowska, D., Colding, C., Wang, J. 2015. Dynamics and Stabilization of the Human Gut Microbiome during the First Year of Life. Cell Host and Microbe, 17(6):852.
Baral, M., Adams, J. B., Geis, E., Mitchell, J., Ingram, J., Hensley, A., Zappia, I., Newmark, S., Gehn, E., Rubin, R. A., Mitchell, K., Bradstreet, J., El-Dahr, J. 2009. Safety and efficacy of oral DMSA therapy for children with autism spectrum disorders: Part B - Behavioral results. BMC Clinical Pharmacology, 9(1):17.
Bent, S., Bertoglio, K., Ashwood, P., Nemeth, E., Hendren, R. L. 2012. Brief Report: Hyperbaric Oxygen Therapy (HBOT) in Children with Autism Spectrum Disorder: A Clinical Trial. Journal of Autism and Developmental Disorders, 42(6):1127–1132.
Browne, H. P., Forster, S. C., Anonye, B. O., Kumar, N., Neville, B. A., Stares, M. D., Goulding, D., Lawley, T. D. 2016. Culturing of ‘unculturable’ human microbiota reveals novel taxa and extensive sporulation. Nature, 533(7604):543–546.
De Angelis, M., Francavilla, R., Piccolo, M., De Giacomo, A., Gobbetti, M. 2015. Autism spectrum disorders and intestinal microbiota. Gut Microbes, 6(3):207–213.
De Angelis, M., Piccolo, M., Vannini, L., Siragusa, S., De Giacomo, A., Serrazzanetti, D. I., Cristofori, F., Guerzoni, M. E., Gobbetti, M., Francavilla, R. 2013. Fecal Microbiota and Metabolome of Children with Autism and Pervasive Developmental Disorder Not Otherwise Specified. PLoS ONE, 8(10):e76993.
Derrien, M., Van Baarlen, P., Hooiveld, G., Norin, E., Müller, M., de Vos, W. M. 2011. Modulation of Mucosal Immune Response, Tolerance, and Proliferation in Mice Colonized by the Mucin-Degrader Akkermansia muciniphila. Frontiers in Microbiology, 2:166.
Donohoe, D. R., Garge, N., Zhang, X., Sun, W., O’Connell, T. M., Bunger, M. K., Bultman, S. J. 2011. The Microbiome and Butyrate Regulate Energy Metabolism and Autophagy in the Mammalian Colon. Cell Metabolism, 13(5):517–526.
Eckburg, P. B. 2005. Diversity of the Human Intestinal Microbial Flora. Science, 308(5728):1635–1638.
Erny, D., de Angelis, A. L. H., et al. 2015. Host microbiota constantly control maturation and function of microglia in the CNS. Nature Neuroscience, 18(7):965–977.
Everard, A., Belzer, C., Geurts, L., Ouwerkerk, J. P., Druart, C., Bindels, L. B., Guiot, Y., Derrien, M., Muccioli, G. G., Delzenne, N. M., de Vos, W. M., Cani, P. D. 2013. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proceedings of the National Academy of Sciences, 110(22):9066–9071.
Gensollen, T., Iyer, S. S., Kasper, D. L., Blumberg, S. 2016. How colonization by microbiota in early life shapes the immune system. Science, 352(6285):539–544.
Gilbert, K., Arseneault-Bréard, J., Monaco, F. F., Beaudoin, A., Bah, T. M., Tompkins, T. A., Godbout, R., Rousseau, G. 2013. Attenuation of post-myocardial infarction depression in rats by n-3 fatty acids or probiotics starting after the onset of reperfusion. British Journal of Nutrition, 109(1):50–56.
Gondalia, S. V., Palombo, E. A., Knowles, S. R., Cox, B., Meyer, D., Austin, D. W. 2012. Molecular Characterisation of Gastrointestinal Microbiota of Children With Autism (With and Without Gastrointestinal Dysfunction) and Their Neurotypical Siblings. Autism Research, 5(6):419–427.
Grimaldi, R., Gibson, G. R., Vulevic, J., Giallourou, N., Castro-Mejía, J. L., Hansen, L. H., Gibson, E. L., Nielsen, D. S., Costabile, A. 2018. A prebiotic intervention study in children with autism spectrum disorders (ASDs). Microbiome, 6(1):133.
Grossi, E., Melli, S., Dunca, D., Terruzzi, V. 2016. Unexpected improvement in core autism spectrum disorder symptoms after long-term treatment with probiotics. SAGE Open Medical Case Reports, 4.
Ho, L. K. H., Tong, V. J. W., Syn, N., Nagarajan, N., Tham, E. H., Tay, S. K., Shorey, S., Tambyah, P. A., Law, E. C. N. 2020. Gut microbiota changes in children with autism spectrum disorder: a systematic review. Gut Pathogens, 12(1):6.
Iovene, M. R., Bombace, F., Maresca, R., Sapone, A., Iardino, P., Picardi, A., Marotta, R., Schiraldi, C., Siniscalco, D., Serra, N., de Magistris, L., Bravaccio, C. 2017. Intestinal Dysbiosis and Yeast Isolation in Stool of Subjects with Autism Spectrum Disorders. Mycopathologia, 182(3-4):349–363.
James, S., Williams, K., Silove, N., Stevenson, S. W. 2015. Chelation for autism spectrum disorder (ASD). Cochrane Database of Systematic Reviews, 11(5):CD010766.
Jandhyala, S. M. 2015. Role of the normal gut microbiota. World Journal of Gastroenterology, 21(29):8787.
Johnsen, P. H., Hilpüsch, F., Cavanagh, J. P., Leikanger, I. S., Kolstad, C., Valle, P. C., Goll, R. 2018. Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: a double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. The Lancet Gastroenterology and Hepatology, 3(1):17–24.
Juge, N., Tailford, L., Owen, C. D. 2016. Sialidases from gut bacteria: a mini-review. Biochemical Society Transactions, 44(1):166–175.
Kang, D.-W., Adams, J. B., Coleman, D. M., Pollard, E. L., Maldonado, J., McDonough-Means, S., Caporaso, J. G., Krajmalnik-Brown, R. 2019. Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota. Scientific Reports, 9(1):5821.
Kang, D.-W., Adams, J. B., et al. 2017. Microbiota Transfer Therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome, 5(1):10.
Kang, D.-W., Adams, J. B., Vargason, T., Santiago, M., Hahn, J., Krajmalnik-Brown, R. 2020. Distinct Fecal and Plasma Metabolites in Children with Autism Spectrum Disorders and Their Modulation after Microbiota Transfer Therapy. mSphere, 5(5):1–17.
Kang, D.-W., Ilhan, Z. E., Isern, N. G., Hoyt, D. W., Howsmon, D. P., Shaffer, M., Lozupone, C. A., Hahn, J., Adams, J. B., Krajmalnik-Brown, R. 2018. Differences in fecal microbial metabolites and microbiota of children with autism spectrum disorders. Anaerobe, 49:121–131.
Kelly, J. R., Minuto, C., Cryan, J. F., Clarke, G., Dinan, T. G. 2017. Cross Talk: The Microbiota and Neurodevelopmental Disorders. Frontiers in Neuroscience, 11.
Kent, J. M., Kushner, S., Ning, X., Karcher, K., Ness, S., Aman, M., Singh, J., Hough, D. 2013. Risperidone Dosing in Children and Adolescents with Autistic Disorder: A Double-Blind, Placebo-Controlled Study. Journal of Autism and Developmental Disorders, 43(8):1773–1783.
Khanna, S., Vazquez-Baeza, Y., González, A., Weiss, S., Schmidt, B., Muñiz-Pedrogo, D. A., Rainey, J. F., Kammer, P., Nelson, H., Sadowsky, M., Khoruts, A., Farrugia, S. L., Knight, R., Pardi, D. S., Kashyap, P. C. 2017. Changes in microbial ecology after fecal microbiota transplantation for recurrent C. difficile infection affected by underlying inflammatory bowel disease. Microbiome, 5(1):55.
Kushak, R. I., Buie, T. M., Murray, K. F., Newburg, D. S., Chen, C., Nestoridi, E., Winter, H. S. 2016. Evaluation of Intestinal Function in Children with Autism and Gastrointestinal Symptoms. Journal of Pediatric Gastroenterology and Nutrition, 62(5):687–691.
Lawley, T. D., Walker, A. W. 2013. Intestinal colonization resistance. Immunology, 138(1):1–11.
Li, M., Liang, P., Li, Z., Wang, Y., Zhang, G., Gao, H., Wen, S., Tang, L. 2015. Fecal microbiota transplantation and bacterial consortium transplantation have comparable effects on the re-establishment of mucosal barrier function in mice with intestinal dysbiosis. Frontiers in Microbiology, 6.
Luo, W., Zhang, F., Shi, Y., Fan, Z., Ji, G. 2012. Should We Standardize the 1,700-Year-Old Fecal Microbiota Transplantation? American Journal of Gastroenterology, 107(11):1755.
Lyte, M. 2013. Microbial Endocrinology in the Microbiome-Gut-Brain Axis: How Bacterial Production and Utilization of Neurochemicals Influence Behavior. PLoS Pathogens, 9(11):e1003726.
Magwira, C. A., Kullin, B., Lewandowski, S., Rodgers, A., Reid, S. J., Abratt, V. R. 2012. Diversity of faecal oxalate-degrading bacteria in black and white South African study groups: insights into understanding the rarity of urolithiasis in the black group. Journal of Applied Microbiology, 113(2):418–428.
Mohajeri, M. H., Fata, G. L., Steinert, R. E., Weber, P. 2018. Relationship between the gut microbiome and brain function. Nutrition Reviews, 76(7):481–496.
Mohamadkhani, A. 2018. Gut Microbiota and Fecal Metabolome Perturbation in Children with Autism Spectrum Disorder. Middle East Journal of Digestive Diseases, 10(4):205–212.
Nylund, L., Nermes, M., Isolauri, E., Salminen, S., de Vos, W. M., Satokari, R. 2015. Severity of atopic disease inversely correlates with intestinal microbiota diversity and butyrate-producing bacteria. Allergy, 70(2):241–244.
Peng, Z., Xiang, J., He, Z., Zhang, T., Xu, L., Cui, B., Li, P., Huang, G., Ji, G., Nie, Y., Wu, K., Fan, D., Zhang, F. 2016. Colonic transendoscopic enteral tubing: A novel way of transplanting fecal microbiota. Endoscopy International Open, 4(6):610–613.
Rossignol, D. A., Bradstreet, J. J., Van Dyke, K., Schneider, C., Freedenfeld, S. H., O’Hara, N., Cave, S., Buckley, J. A., Mumper, E. A., Frye, R. E. 2012. Hyperbaric oxygen treatment in autism spectrum disorders. Medical Gas Research, 2(1):16.
Rossignol, D. A., Frye, R. E. 2012. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Molecular Psychiatry, 17(3):290–314.
Saha, Butler, V., Neu, H., Lindenbaum, J. 1983. Digoxin-inactivating bacteria: identification in human gut flora. Science, 220(4594):325–327.
Sampanthavivat, M., Singkhwa, W., Chaiyakul, T., Karoonyawanich, S., Ajpru, H. 2012. Hyperbaric oxygen in the treatment of childhood autism: a randomised controlled trial. Diving and Hyperbaric Medicine, 42(3):128–133.
Santocchi, E., Guiducci, L., et al. 2020. Effects of Probiotic Supplementation on Gastrointestinal, Sensory and Core Symptoms in Autism Spectrum Disorders: A Randomized Controlled Trial. Frontiers in Psychiatry, 11.
Schreibman, L., Dawson, G., Stahmer, A. C., Landa, R., Rogers, S. J., McGee, G. G., Kasari, C., Ingersoll, B., Kaiser, A. P., Bruinsma, Y., McNerney, E., Wetherby, A., Halladay, A. 2015. Naturalistic Developmental Behavioral Interventions: Empirically Validated Treatments for Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 45(8):2411–2428.
Shaaban, S. Y., Gendy, Y. G. E., Mehanna, N. S., El-Senousy, W. M., El-Feki, H. S. A., Saad, K., El-Asheer, O. M. 2018. The role of probiotics in children with autism spectrum disorder: A prospective, open-label study. Nutritional Neuroscience, 21(9):676– 681.
Singh, K., Connors, S. L., Macklin, E. A., Smith, K. D., Fahey, J. W., Talalay, P., Zimmerman, A. W. 2014. Sulforaphane treatment of autism spectrum disorder (ASD). Proceedings of the National Academy of Sciences, 111(43):15550–15555.
Strati, F., Cavalieri, D., Albanese, D., De Felice, C., Donati, C., Hayek, J., Jousson, O., Leoncini, S., Renzi, D., Calabrò, A., De Filippo, C. 2017. New evidences on the altered gut microbiota in autism spectrum disorders. Microbiome, 5(1):24.
Sturman, N., Deckx, L., van Driel, M. L. 2017. Methylphenidate for children and adolescents with autism spectrum disorder. Cochrane Database of Systematic Reviews, 11(11):CD011144.
Surawicz, C. M., Brandt, L. J., Binion, D. G., Ananthakrishnan, A. N., Curry, S. R., Gilligan, P. H., McFarland, L. V., Mellow, M., Zuckerbraun, B. S. 2013. Guidelines for Diagnosis, Treatment, and Prevention of Clostridium difficile Infections. American Journal of Gastroenterology, 108(4):478–498.
Swanson, P. A., Kumar, A., Samarin, S., Vijay-Kumar, M., Kundu, K., Murthy, N., Hansen, J., Nusrat, A., Neish, A. S. 2011. Enteric commensal bacteria potentiate epithelial restitution via reactive oxygen species-mediated inactivation of focal adhesion kinase phosphatases. Proceedings of the National Academy of Sciences, 108(21):8803–8808.
Thomas, R. H., Meeking, M. M., Mepham, J. R., Tichenoff, L., Possmayer, F., Liu, S., MacFabe, D. F. 2012. The enteric bacterial metabolite propionic acid alters brain and plasma phospholipid molecular species: further development of a rodent model of autism spectrum disorders. Journal of Neuroinflammation, 9(1):695.
Tian, H., Ding, C., Gong, J., Ge, X., McFarland, L. V., Gu, L., Wei, Y., Chen, Q., Zhu, W., Li, J., Li, N. 2016. Treatment of Slow Transit Constipation With Fecal Microbiota Transplantation. Journal of Clinical Gastroenterology, 50(10):865–870.
Vindigni, S. M., Surawicz, C. M. 2016. Stool transplant for the senior citizen: Is it safe? Maturitas, 88:23–24.
Vindigni, S. M., Surawicz, C. M. 2017. Fecal Microbiota Transplantation. Gastroenterology Clinics of North America, 46(1):171–185.
Wang, L., Christophersen, C. T., Sorich, M. J., Gerber, J. P., Angley, M. T., Conlon, M. A. 2013. Increased abundance of Sutterella spp. and Ruminococcus torques in feces of children with autism spectrum disorder. Molecular Autism, 4(1):42.
Wang, S., Xu, M., Wang, W., Cao, X., Piao, M., Khan, S., Yan, F., Cao, H., Wang, B. 2016. Systematic Review: Adverse Events of Fecal Microbiota Transplantation. Plos One, 11(8):e0161174.
Wrzosek, L., Miquel, S., Noordine, M.-L., et al. 2013. Bacteroides thetaiotaomicron and Faecalibacterium prausnitzii influence the production of mucus glycans and the development of goblet cells in the colonic epithelium of a gnotobiotic model rodent. BMC Biology, 11(1):61.
Xiong, Y., Miyamoto, N., Shibata, K., Valasek, M. A., Motoike, T., Kedzierski, R. M., Yanagisawa, M. 2004. Short-chain fatty acids stimulate leptin production in adipocytes through the G protein-coupled receptor GPR41. Proceedings of the National Academy of Sciences, 101(4):1045–1050.
Xu, J. 2003. A Genomic View of the Human-Bacteroides thetaiotaomicron Symbiosis. Science, 299(5615):2074–2076.
Zhang, F., Amateau, S. K., Khashab, M. A., Okolo, P. I. 2012. Mid-gut stents. Current Opinion in Gastroenterology, 28(5):451–460.
Zhang, F., Cui, B., He, X., Nie, Y., Wu, K., Fan, D. 2018. Microbiota transplantation: concept, methodology and strategy for its modernization. Protein and Cell, 9(5):462–473.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.