Abstract
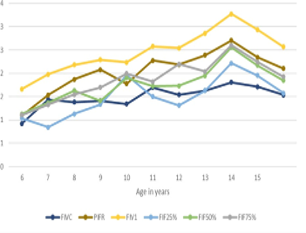
The prevalence of lung diseases is increasing globally. Mortality, morbidity and respiratory disability are a growing health concern. The pulmonary function test is an accurate tool for detecting airway and lung abnormalities. Early diagnosis of respiratory disease is key to preventing mortality and morbidity. The current study has evaluated the relation of the anthropometric parameters and inspiratory parameters of pulmonary function test and also analyzed its behaviour over the growing age in Indian children. The current study included 2109 school-aged children aged 6 to 15. The height, weight, body mass index and body surface area were recorded. The spirometry was performed in accordance with the protocols. The parameters of the inspiratory flow volume loop were recorded. This study observed a good relation between the anthropometric parameters and inspiratory lung function parameters and the parameters were higher in males than in females. The behaviour of these parameters at various points of growing age was analyzed. This study revealed geographical, gender wise variation in the inspiratory parameters. The study also revealed different patterns of lung growth in boys and girls. Hence this study recommends to include inspiratory parameter assessment in the routine assessment of respiratory patients for early and accurate diagnosis of lung pathology in young children.
Full text article
References
American Thoracic Society 1995. Standardization of Spirometry, 1994 Update. American Thoracic Society. American Journal of Respiratory and Critical Care Medicine, 152(3):1107–1136.
Dickman, M. L., Schmidt, C. D., Gardner, R. M. 1971. Spirometric standards for normal children and adolescents (ages 5 years through 18 years). American Review of Respiratory Disease, 104(5):680–687.
Ghosh, S., Ohar, J. A., Drummond, M. B. 2017. Peak Inspiratory Flow Rate in Chronic Obstructive Pulmonary Disease: Implications for Dry Powder Inhalers. Journal of Aerosol Medicine and Pulmonary Drug Delivery, 30(6):381–387.
Grivas, T. B., Burwell, R. G., Purdue, M., Webb, J. K., Moulton, A. 1991. A segmental analysis of thoracic shape in chest radiographs of children. Changes related to spinal level, age, sex, side and significance for lung growth and scoliosis. Journal of Anatomy, 178:21–38.
Guyton, A. C., Hau, J. E. 2006. Pulmonary ventilation. In: Textbook of medical physiology. 11th Ed., India: W.B. Saunders Company, P.471-482. ISBN: 978-8131218013.
Hibbert, M. E., Couriel, J. M., Landau, L. I. 1984. Changes in lung, airway, and chest wall function in boys and girls between 8 and 12 yr. Journal of Applied Physiology, 57(2):304–308.
Khadgawat, R., Marwaha, R. K., Mehan, N., Surana, V., Dabas, A., Sreenivas, V., Gaine, M. A., Gupta, N. 2016. Age of onset of puberty in apparently healthy school girls from northern India. Indian Pediatrics, 53(5):383–387.
Khadilkar, V. V., Stanhope, R. G. 2006. Secular trends in puberty. Indian Pediatrics, 43(6):475–478.
Koopman, M., Zanen, P., Kruitwagen, C. L., van der Ent, C. K., Arets, H. G. 2011. Reference values for paediatric pulmonary function testing: The Utrecht dataset. Respiratory Medicine, 105(1):15–23.
Mahler, D. A. 2019. Peak Inspiratory Flow Rate: An Emerging Biomarker in Chronic Obstructive Pulmonary Disease. American Journal of Respiratory and Critical Care Medicine, 199(12):1577–1579.
Modrykamien, A. M., Gudavalli, R., Mccarthy, K., Liu, X., Stoller, J. K. 2009. Detection of upper airway obstruction with spirometry results and the flow-volume loop: a comparison of quantitative and visual inspection criteria. Respiratory Care, 54(4):474–479.
Nair, R. H., Kesavachandran, C., Sanil, R., Sreekumar, R., Shashidhar, S. 1997. Prediction equation for lung functions in South Indian children. Indian Journal of Physiology and Pharmacology, 41(4):390–396.
Owens, G. R., et al. 1983. Spirometric Diagnosis of Upper Airway Obstruction. Archives of Internal Medicine, 143(7):1331.
Quanjer, P. H., Borsboom, G. J. J. M., Kivastik, J., Merkus, P. J. F. M., Hankinson, J. L., Houthuijs, D., Brunekreef, B., Ihorst, G., Kühr, J. 2008. Cross-sectional and longitudinal spirometry in children and adolescents: interpretative strategies. American Journal of Respiratory and Critical Care Medicine, 178(12):1262–1270.
Rajkumar, P., Pattabi, K., Vadivoo, S., Bhome, A., Brashier, B., Bhattacharya, P., Mehendale, S. M. 2017. A cross-sectional study on prevalence of chronic obstructive pulmonary disease (COPD) in India: rationale and methods. BMJ Open, 7(5):e015211.
Rosenthal, M., Bain, S. H., Cramer, D., Helms, P., Deni- son, D., Bush, A., Warner, J. O. 1993. Lung function in white children aged 4 to 19 years: I–Spirometry. Thorax, 48(8):794–802.
Salvi, S., Kumar, G. A., Dhaliwal, R. S., Paulson, K., Agrawal, A., Koul, P. A., Mahesh, P. A., Nair, S., Singh, V., Aggarwal, A. N., Christopher, D. J., Guleria, R., Mohan, B. V. M., Tripathi, S. K., Ghoshal, A. G., Kumar, R. V., Mehrotra, R., Shukla, D. K., Dutta, E., Dandona, L. 2018. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. The Lancet Global Health, 6(12):1363–1374.
Schrader, P. C., Quanjer, P. H., Zomeren, B. C. V., Wise, M. E. 1984. Changes in the FEV1-height relationship during pubertal growth. Bulletin Europeen de Physiopathologie Respiratoire, 20(4):381–388.
Sliman, N. A., Dajani, B. M., Shubair, K. S. 1982. Pulmonary function in normal Jordanian children. Thorax, 37(11):854–857.
Sterner, J. B., Morris, M. J., Sill, J. M., Hayes, J. A. 2009. Inspiratory flow-volume curve evaluation for detecting upper airway disease. Respiratory Care, 54(4):461–466.
Sudeep, K., Mangala, D., Sandip, C. 2021. Prediction Model for Peak Expiratory Flow Rate in Rural Indian Girls. International Journal of Pharma and Bio Sciences, 12(2):68–72.
Vilozni, D., Efrati, O., Barak, A., Yahav, Y., Augarten, A., Bentur, L. 2009. Forced inspiratory flow volume curve in healthy young children. Pediatric Pulmonology, 44(2):105–111.
Visser, F. J., Ramlal, S., Pelzer, B., Dekhuijzen, P. R., Heijdra, Y. F. 2010. Random variation of inspiratory lung function parameters in patients with COPD: a diagnostic accuracy study. BMC Pulmonary Medicine, 10(1).
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.