Abstract
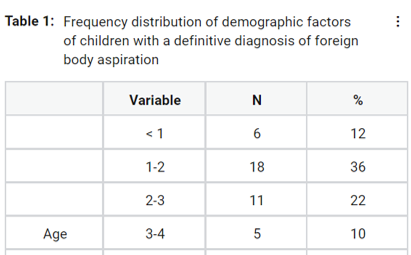
Foreign body aspiration is still one of the most important diagnostic and therapeutic items for physicians. The mortality rate and prevalence of diseases caused by foreign bodies are higher in children due to the relatively narrow airway and immature protective mechanisms. Considering the high prevalence of foreign body aspiration in children, as well as the possible complications, we decided to investigate the frequency distribution of signs and symptoms in children with foreign body aspiration. This retrospective cross-sectional study was performed on the files of 50 children with foreign body aspiration who referred to Khatam Al-Anbia Hospital in Zahedan, Iran from 2016 to 2018. The files were entered into the study by the census method, based on inclusion and exclusion criteria. Finally, demographic factors (age and sex), as well as the type of aspirated object, signs, and symptoms, were examined. The files of 50 children with a foreign body aspiration were reviewed. Among the patients, 27 (54%) were boys and 23 (46%) were girls. The highest frequency was between 1 and 2 years, with 36%. The most common symptom in these patients was cough and respiratory distress with a frequency of 72% and the most common clinical findings were unilateral wheezing with 50% and decreased unilateral respiratory sounds with 18%. Also, the most common types of foreign objects were nuts with a frequency of 44% and supari with 38%. Also, unilateral wheezing had a significant relationship with the type of aspirated foreign body (P = 0.01). Children between the ages of one and two years are more likely to have foreign body aspiration, and in children with symptoms of cough and respiratory distress, as well as clinical findings of unilateral wheezing and decreased unilateral respiratory sounds, foreign body aspiration should be suspected.
Full text article
References
Adjeso, T., Damah, M. C., Murphy, J. P., Anyomih, T. T. K. 2017. Foreign Body Aspiration in Northern Ghana: A Review of Pediatric Patients. International Journal of Otolaryngology, 2017:1–4.
Ahmed, A. A. O., Shuiabu, I. Y. 2014. Inhaled foreign bodies in a paediatric population at AKTH Kano Nigeria. Nigerian Medical Journal, 55(1):77–82.
Alshehri, K. A., Alharbi, A. A., Yaghmoor, B. E., Salman, A. K., Alaydarous, S. A., Abdalwassie, L. K., Mosli, M. H., Marzouki, H. Z. 2019. Awareness of the first aid management of foreign body aspiration among students: A cross-sectional study. Journal of Education and Health Promotion, 8:220– 220.
Aslan, N., Yıldızdaş, D., Özden, Ö., Yöntem, A., Horoz, Ö. Ö., Kılıç, S. 2019. Evaluation of foreign body aspiration cases in our pediatric intensive care unit: A single-centre experience. Turkish Archives of Pediatrics/Türk Pediatri Arşivi, 54(1):44–48.
Behrman, R. E., Kliegman, R., Jenson, H. 2007. Behrman: Nelson textbook of pediatrics. 18th edition. Philadelphia, Pa: WB Saunders. ISBN: 9781437721805. 3200pg.
Bhananker, S. M., Harless, J., Ramaiah, R. 2014. Pediatric airway management. International Journal of Critical Illness and Injury Science, 4(1):65–70.
Cichero, J. 2018. Age-Related Changes to Eating and Swallowing Impact Frailty: Aspiration, Choking Risk, Modified Food Texture and Autonomy of Choice. Geriatrics, 3(4):69–69.
Cramer, N., Jabbour, N., Tavarez, M. M., Taylor, R. S. 2018. Foreign body aspiration. StatPearls Publishing.
Ding, G., Wu, B., Vinturache, A., Cai, C., Lu, M., Gu, H. 2020. Tracheobronchial foreign body aspiration in children: A retrospective single-center crosssectional study. Medicine, 99(22):20480–20480.
Dodson, H., Cook, J. 2020. Foreign Body Airway Obstruction (FBAO). StatPearls Publishing.
Farzizadeh, M., Hashemian, H., Atrkar-Roshan, Z. 2013. Clinical and radiographic findings of foreign body aspiration in children admitted to 17- Shahrivar hospital in Rasht during 1996-2008. KAUMS Journal (FEYZ), 17(5):495–500.
Foltran, F., Ballali, S., Rodriguez, H., van As, A. B. S., Passali, D., Gulati, A., Gregori, D. 2013. Inhaled foreign bodies in children: A global perspective on their epidemiological, clinical, and preventive aspects. Pediatric Pulmonology, 48(4):344–351.
Ganie, F. A., Wani, M. L., Ahangar, A. G., Lone, G. N., Singh, S., Lone, H., Wani, S. N. 2014. The efficacy of rigid bronchoscopy for foreign body aspiration. Bulletin of Emergency & Trauma, 2(1):52–54.
Haddadi, S., Marzban, S., Nemati, S. 2015. Tracheobronchial foreign-bodies in children; a 7 year retrospective study. Iranian journal of Otorhinolaryngology, 27(82):377–385.
Idris, S., Murphy, R. A., Witmans, M., El-Hakim, H. 2018. A simple management option for chronically impacted sharp tracheobronchial foreign bodies in children. Journal of Otolaryngology - Head & Neck Surgery, 47(1):26.
Janahi, I. A., Khan, S., Chandra, P., Al-Marri, N., Saadoon, A., Al-Naimi, L., Al-Thani, M., Greer, W. 2017. A new clinical algorithm scoring for management of suspected foreign body aspiration in children. BMC Pulmonary Medicine, 17(1):61–61.
Kalyanappagol, V. T., Kulkarni, N., Bidri, L. 2007. Management of tracheobronchial foreign body aspirations in paediatric age group-A 10-year retrospective analysis. Indian Journal of Anaesthesia, 51(1):20–23.
Kazemi, S., Savabi, G., Khazaei, S., Savabi, O., Esmaillzadeh, A., Keshteli, A. H., Adibi, P. 2011. Association between food intake and oral health in elderly: Sepahan systematic review no. 8. Dental research journal, 8(supple 1):15–20.
Kumar, S., Al-Abri, R., Sharma, A., Al-Kindi, H., Mishra, P. 2010. Management of pediatric tracheo bronchial foreign body aspiration. Oman Medical Journal, 25(4):19.
Mahmoud, M., Imam, S., Patel, H., King, M. 2012. Foreign body aspiration of a dental bridge in the left mainstem bronchus. Case reports in medicine, page 4.
Naragund, A. I., Mudhol, R., Harugop, A., Patil, P., Hajare, P., Metgudmath, V. 2014. Tracheobronchial foreign body aspiration in children: a one-year descriptive study. Indian Journal of Otolaryngology and Head & Neck Surgery, 66(supple 1):180–185.
Passali, D., Gregori, D., Lorenzoni, G., Cocca, S., Loglisci, M., Passali, F., Bellussi, L. 2015. Foreign body injuries in children: a review. Acta Otorhinolaryngologica Italica, 35(4):265–271.
Passali, D., Lauriello, M., Bellussi, L., Passali, G., Passali, F., Gregori, D. 2010. Foreign body inhalation in children: an update. Acta Otorhinolaryngologica Italica, 30(1):27–32.
Puja, D., Arun, K. R., Ashok, B., Rathi, S. 2017. Foreign Body Aspiration in Paediatric Airway. International Journal of Medical Research & Health Sciences, 6(3):17–21.
Reid, A., Hinton-Bayre, A., Vijayasekaran, S., Herbert, H. 2020. Ten years of paediatric airway foreign bodies in Western Australia. International Journal of Pediatric Otorhinolaryngology, 129:109760– 109760.
Rose, D., Dubensky, L. 2019. Airway Foreign Bodies. StatPearls Publishing.
Rothmann, B. F., Boeckman, C. R. 1980. Foreign Bodies in the Larynx and Tracheobronchial Tree in Children. Annals of Otology, Rhinology & Laryngology, 89(5):434–436.
Salih, A. M., Alfaki, M., Alam-Elhuda, D. M. 2016. Airway foreign bodies: A critical review for a common pediatric emergency. World journal of emergency medicine, 7(1):5–12.
Schweiger, C., Cohen, A. P., Rutter, M. J. 2016. Tracheal and bronchial stenoses and other obstructive conditions. Journal of Thoracic Disease, 8(11):3369–3378.
Sultan, T. A., van As, A. B. 2016. Review of tracheobronchial foreign body aspiration in the South African paediatric age group. Journal of Thoracic Disease, 8(12):3787–3796.
Xu, Y., Feng, R. L., Jiang, L., Ren, H. B., Li, Q. 2018. Correlative factors for the location of tracheobronchial foreign bodies in infants and children. Journal of Thoracic Disease, 10(2):1037–1042.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.