Importance of mental peace for physical well-being among medical and dental personnel during a pandemic - An awareness-based study
Abstract
The connection between the body and the mind is an intangible one. The health of one affects the other, and so does the illness. Mental peace is intimately connected to physical health. Aim of the study is to address the mental health of the health workers and factors which influence them to improve their knowledge and maintain their physical well-being and thus improve the quality of work and successfully fulfilling their duties as medical personnel. Health workers should be provided with psychosocial support which will help them. Chronic levels of stress lead to unhealthy coping methods. Organisations and agencies that the medical personnel work under should provide relief efforts to obtain the effectiveness of the workforce. A cross-sectional survey was conducted among medical and dental personnel through a questionnaire consisting of 15 questions and is circulated among the target population. The sample size of the survey was 100 and obtained from medical personnel, including dentists, physicians and surgeons. 70.5% were aware that mental peace is important for physical well-being. According to the results, mental health has to be improved for 36.3% and for 63.7% it was good. More population of dentists suffered from panic and anxiety-related disorders due to the current crisis, and they strongly agreed that mental peace is essential for physical well-being. This study concludes that the medical personnel have poor mental health during this pandemic which is affecting their physical health also and vice versa.
Keywords
COVID-19, mental peace, poor health, medical personnel, physical wellness
Introduction
Mental health is an integral part of health which is intimately connected with physical health (Ghebreyesus, 2020). Health professionals working to treat a deadly disease in a pandemic are surrounded by a complex environment. They tend to have high-level stress that gradually shows symptoms of PTSD (post-traumatic stress disorder) which causes decreased efficiency in work. Chronic stress leads to immune suppression that causes chronic illness and behavioural changes.
Health workers should be provided with psychosocial support which will help them. Chronic levels of stress lead to unhealthy coping methods. Organisations and agencies that the medical personnel work under should provide relief efforts to obtain the effectiveness of the workforce (Surya, Jaff, Stilwell, & Schubert, 2017). The health workers should be protected, which will increase their motivation. The willingness to work is influenced by threat and efficacy. The government should also support healthcare workers, which gives mental support to them (Imai et al., 2010).
Trauma exposure which is continual has an effect on occupational mental health. Employers should prepare workers for their occupational exposure to trauma which affects mental health and support the health care workers constantly (Connorton, Perry, Hemenway, & Miller, 2012). Health organisations and the government should help the medical personnel during a pandemic crisis. Aim of the study is to address the mental health of the health workers and factors which influence them to improve their knowledge and maintain their physical well-being and thus improve the quality of work and successfully fulfilling their duties as medical personnel.
Materials and Methods
A descriptive study was done among medical and dental personnel. The study protocol was approved by the institutional review board. The sample size of the survey was 100 and obtained from medical personnel. The questionnaire was distributed online by google forms. The questionnaire consisted of 15 questions which were predominantly close-ended. Survey results were validated, and the data was collected according to respondents. Random sampling was used. Socio-demographic results were analysed using descriptive statistics, and the association between variables were analysed using the chi-square test and the use of statistical software named SPSS, which was used for collection and interpretation of data collected.
Results and Discussion
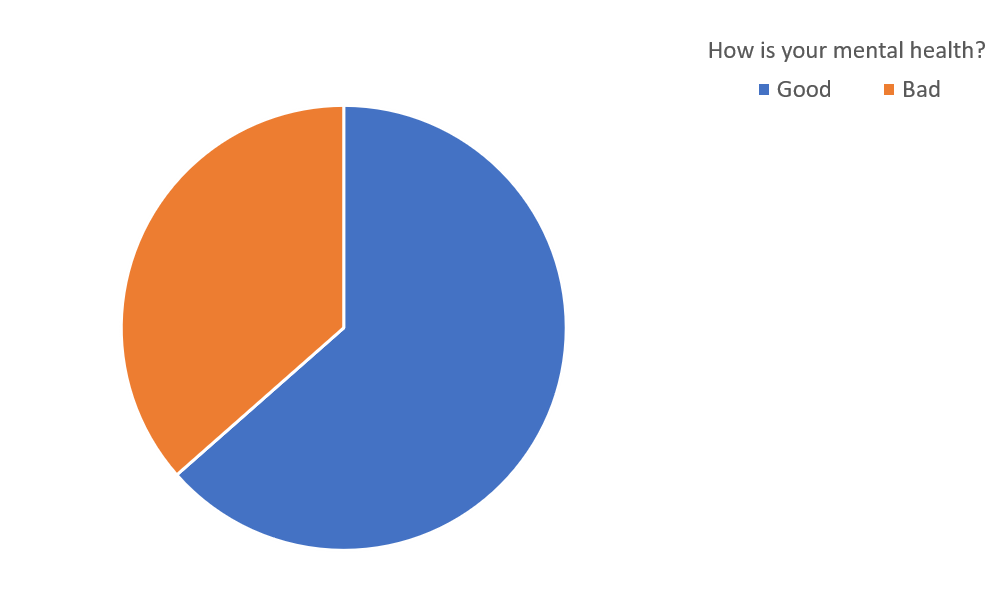
A total of 133 participated in the study in which 55.4% were female, and the remaining 44.6% were male (Figure 1). In this study, there were 33.6% physicians, 14.2% were surgeons, and 52.2% were dentists (Figure 2). 36.6% told they had bad mental health, and 63.7% were having a good mental health (Figure 3). When asked about the quality of sleep, 66.7% had a good sleep, whereas 33.3% tend to wake up in between (Figure 4). 67.3% had a fear of spreading the infection to family members, where 32.7% disapproved (Figure 5).


















70.8% of the workers had access to personal protective equipment, whereas the remaining didn't have access to PPE (Figure 6). 55.4% feel there is an increase in anxiety level, while 44.6% disapproves (Figure 7). The health organisation in which the doctor's practice was 63.7% is being protected and supported (Figure 8). 61% feel they have been isolated by family and society (Figure 9). 73.5% have taken steps to reduce stress and anxiety by yoga and exercises (Figure 10). 70.8% have already had experience treating a deadly disease (Figure 11). The age of the participants was 70.8% between the age 25-30, 16.8% between the age 30-40 and 12.4% were 40 and above (Figure 12). 62.8% have experienced the symptoms of COVID-19 (Figure 13). 79.6% feels there is a relationship between mental and physical health (Figure 14). 70.5% aware that mental peace is important for physical well-being (Figure 15). The following bar charts represent the association between profession and parameters like age, gender, anxiety and importance of mental peace. 113 participated in this study were 33.6% physicians, 14.2% surgeons and 52.2% were dentists.
In Figure 16, Age group of 25-30 years is the most common (p value- .005 (<0.05) hence its significant. In Figure 17, Majority are female participants. p value- 0.31(> 0.05) hence not significant. In Figure 18, Majority of participants are dentists, and they believe that mental peace is very essential for physical appearance. P value- 0.00 (<0.5) hence its significant. In Figure 19, Dentists are the mostly experiencing anxiety in the recent times. (p value - 0.02 (<0.05) hence its significant)
The mental health has to be improved for 36.3% and 63.7% it was good. This is quite a normal experience for medical personnel under pressure managing mental health is very important as managing mental health is very important as managing physical health (Imai et al., 2010). The quality of sleep was 66.7% good, whereas 33.3% would wake up in between. More than a third of the population suffers from insomnia and sleeplessness, which causes burnout and increases the need for medical personnel (Singh, Sharda, Gautam, & Hawa, 2020). The fear of spreading the infection to family members among the doctors is 67.3%. 70.8% have access to personal protective equipment. Health care workers totally rely on PPE, and there is a rising demand due to limited access to supplies and mounting disruption (Mahmood, Crimbly, Khan, Choudry, & Mehwish, 2020). 55.4% experienced an increase in anxiety. Adverse physiological outcomes occur due to excessive workloads. The inadequate PPE and infection rate may also be the reason for stress among medical staff (Spoorthy, Pratapa, & Mahant, 2020). 63.7% are being protected and supported by the health organisation they are working for. Health organisations support by providing access to counselling and psychiatry and helping them with workload management. They should also be provided with adequate PPE kit and regular praise (Walton, Murray, & Christian, 2020). 61.1% are isolated from family and society. 73.5% take steps to reduce stress and anxiety by doing yoga and exercises. Providing frequent shift systems, counselling, and medical advice will reduce pressure (Rana, Mukhtar, & Mukhtar, 2020). 70.8% have experience treating deadly disease before. 62.8% have experienced symptoms of COVID-19. 79.6% feels that there is a strong relationship between mental and physical health. There is a strong link between mental and physical health which shows direct and indirect effects. It has an influence of past mental health on physical health and vice versa (Ohrnberger, Fichera, & Sutton, 2017). Previously we have worked on many topics on tooth-related studies which have led us to work on the current topic. It is concluded that oral lesions do not play many roles in relating to stress and other psychological diseases. Schizophrenia could be a common disorder during which saliva secretion is distributed as a result of antipsychotic pharmacotherapy. Stress can increase empathy which can cause pro-social behaviour among people and also psychological stress (Prasanna & Gheena, 2016). Diagnostic research studies are often time-consuming and may affect the pathologist and cause extreme stress due to lack of expertise or unavailability of facilities (Shree et al., 2019). Age of the individuals also reduces the threshold of stress (Palati et al., 2020).
When a surgical specimen handover is done from an operation theatre to a laboratory there has been immense stress and fatigue among people and doctors (Krishnan et al., 2018). The olze’s method for age estimation proves to be a very good, non-invasive, indirect method to estimate the age of an individual if the individual is unable to reveal his or her age due to extreme stress (Abitha & Santhanam, 2019; Palati et al., 2019). Dental photography is an essential part of orthodontic treatment, but the presence of intraoral mirrors have been a main primary cause for the patient's stress (Hannah et al., 2018). Mental health issues like depression and schizophrenia can be caused due to tooth sensitivity or tooth decay or even gum disease (Gunasekaran & Abilasha, 2016). Changes in climate and global warming may require migration of the population which may lead to acculturation stress. Psychological stress is the main risk for periodontal diseases among humans. Molar incisor hypomineralization is a type of enamel defect causing infection, maternal psychological stress which leads to more molar incisor hypomineralization (Sukumaran & Padavala, 2018). Hyperpigmentation of the gingiva can affect the confidence of the patients that results in psychological stress (Manohar & Abilasha, 2019). The oral mucosa is thought to be highly reactive to psychological influences, and in some oral diseases, it may have direct effects on emotions and conflicts (Sheriff & Santhanam, 2018). The stress in a child can cause the child to grind their teeth and hence reduce the tooth height and also cause mental problems (Harrita & Santhanam, 2019). Many studies state that awareness should be created among doctors to be more careful among patients mentally and to stop stress-related disorders among the dentists due to medical negligence (Uma et al., 2020). Thus many such parameters can affect or increase the stress levels in individuals, hence during a pandemic, the emotional support offered to the medical personnel is of utmost importance to prevent them from losing themselves in the situation of a medical crisis.
Conclusion
There is an unequal distribution of sample size; hence the uniformity in the population can yield better results. Reasons for stress are not mentioned in the questionnaire, is a limitation to the study, which may be included in a blinded study. Providing better protection and care can help medical personnel from stress and depression to have good mental health. In our study, we found that medical personnel report poor mental health and the initiatives are taken by the health organisations and themselves to improve their conditions to provide maximum support to the medical field during a pandemic situation.
Conflict of Interest
The authors declare that they have no conflict of interest for this study.
Funding Support
The authors declare that they have no funding support for this study.