The use of an Alpine climate in the treatment of immune thrombocytopenic purpura (ITP) in children of the Kyrgyz Republic
Abstract
The objective of the study is to evaluate the effectiveness of the use of alpine (high-altitude) climatotherapy in the chronic form of immune thrombocytopenia in children. The article presents the results of the treatment of immune thrombocytopenia in children during high altitude climatotherapy. For this type of treatment, the alpine climate of the Tuya-Ashu pass (3200 meters above sea level) in the Kyrgyz Republic used. A 40-day stay in the highlands contributes to the relief of hemorrhagic syndrome and a significant increase in platelet count. Evaluation of the treatment results showed that out of 32 children who received alpine (high-altitude) climatotherapy once, 2 achieved complete and 14 had partial remission. In 11 children, the improvement of clinical and hematological parameters was temporary, and the absence of effect recorded in 5 patients. 50% of children with chronic immune thrombocytopenia (ITP) responded positively to a single course of treatment. Repeated courses of treatment led only to an improvement in clinical and haematological parameters. In our study, we have a case of a complete recovery of a child with immune thrombocytopenia (ITP) after 5 treatments in high altitude conditions.
Keywords
Alpine climatotherapy, Hemorrhagic syndrome, Immune thrombocytopenia (ITP), Kyrgyz Republic, Platelet count, Prednisone, Remission, Splenectomy
Introduction
Immune thrombocytopenic Purpura (ITP) is an autoimmune disease characterized by a decrease in platelet count due to antibody-mediated platelet destruction and damage to megakaryocytes, and as a result, a decrease in platelet production and the development of hemorrhagic syndrome (Audia, Rossato, & Santegoets, 2017; Rodeghiero et al., 2009). The diagnostic level of platelets, indicating thrombocytopenia, is less than 100 × 109 / l (Rodeghiero et al., 2009). Clinically, the severity of the manifestations of hemorrhagic syndrome in children mainly correlates with the severity of thrombocytopenia.
ITP is the most common nosological form of thrombocytopenia of immune origin - approximately 2–4 cases per 100,000 population per year. In adulthood, the incidence of ITP among women about 2 times more often than men, and in childhood, the incidence rate is the same for boys and girls (Terrell et al., 2010). According to international consensus on the study and treatment of ITP, prednisone, dexamethasone or methylprednisolone are equally acceptable as first-line therapy. Intravenous immunoglobulin and anti-Rhesus immunoglobulin (anti ^) are useful for increasing platelet counts, but the effect is usually transient (Neunert et al., 2011). Second-line therapy includes splenectomy, thrombopoietin receptor agonists (romiplostim, eltrombopag), azathioprine, danazol, mycophenolate mofetil, rituximab, cyclosporin A and cyclophosphamide (Bussel et al., 2009; George, 2018; Grainger, Locatelli, & Chotsampancharoen, 2015; Wong et al., 2017). All of them are classified into the drugs that are prescribed once or in one course (splenectomy, rituximab), and drugs that require continuous administration (corticosteroids, immunosuppressants, thrombopoietin receptor agonists).
In the Kyrgyz Republic, the treatment of immune thrombocytopenic purpura (ITP) primarily based on first-line therapy. Intravenous immunoglobulin and anti-Rhesus immunoglobulin (anti ^) have been found useful, but due to the high cost, not prescribed on a large scale. Anti-Rhesus immunoglobulin and thrombopoietin receptor agonists are not registered and not used. Therefore, in the arsenal of haematologists of the country in the treatment of ITP, there remains a limited choice of drugs in the form of prescribing glucocorticosteroids, and in severe cases, splenectomy, which is not entirely desirable in children. In this regard, the search for an alternative and affordable methods of treating ITP in the country is considered relevant.
Since the 1990s (Kyrgyz Republic), an alpine climate actively used in the treatment of ITP in adults, which has shown some effectiveness, and remission achieved in 60% of cases. Given this circumstance, an alpine climate was included in the treatment regimen for children with chronic immune thrombocytopenia (ITP), in cases where there is no effectiveness from first-line drugs. Moreover, today we already have specific positive results, which we decided to state. The objective is to evaluate the effectiveness of the use of high-altitude climatotherapy in the chronic form of immune thrombocytopenia in children.
Materials and Methods
For the period from 2015 to 2019, we analyzed the clinical cases of chronic immune thrombocytopenia (ITP) in children treated in a high-altitude hospital and subsequent follow-up. The study included 32 ITP children, including 17 girls and 15 boys (aged 3 to 14 years; average age 8.4 ± 1.35 years). The duration of the disease ranged from 4 to 8 years. Children came to us with a final diagnosis, after the ineffectiveness of the undertaken treatment with first-line drugs, before the splenectomy. The final diagnosis for children made at the Department of Pediatric Hematology of the National Center for Maternal and Child Welfare and the Interregional Children's Clinical Hospital of Osh region in the Kyrgyz Republic.
The alpine base of the I.K. Akhunbaev Kyrgyz State Medical Academy located on the Tuya-Ashu pass, 3200 meters above sea level, at a distance of 135 km from the capital Bishkek. The climate of the Tuya-Ashu pass changes dramatically during the day: from sunny to cloudy with short-term rains alternating with hail or snow. Summer is usually short (60-75 days); air temperature varies from 17° to 22° heat during the day. The amount of precipitation is almost two times greater than in Bishkek and amounts to 753 mm per year. The alpine base is a single-story building with 40 beds. The building has 15 wards, a treatment room, a ward for medical personnel, a kitchen and a dining room (Figure 1). There are organized high-calorie three meals a day. The duration of the alpine climatotherapy course was 40 days.
In all children, standard blood tests performed before and after alpine climatotherapy. During the stay in the mountains (on the 20th day and by the end of the stay), the platelet count determined using a Penta 80 haematology analyzer (Horiba ABX, 80). Data analysis package of the Microsoft EXCEL 2007 software used to obtain data for getting Statistics. The nature of the variability of the data from laboratory studies obeyed the laws of the normal distribution, which allowed us to reflect the results in the form of the arithmetic mean (M) and mean error of the mean (m). Differences between groups evaluated using Student's t-test for independent samples and the Mann-Whitney U-test (non-parametric method) with a confidence level of 0.05.
Results and Discussion
All children before admission to alpine climatotherapy used various methods of drug therapy, which had temporary effectiveness. So, treatment with hormones, in particular, prednisone in doses of 1-2 mg per kg of body weight, was carried out for 15 children for 20-25 days. Of these, 9 showed a positive short-term effect of 1 to 3 months, the remaining 6 children - from 4 to 6 months. At each subsequent exacerbation, they prescribed only glucocorticosteroids - prednisone.
|
Treatment results |
Alpine climatotherapy |
||||
|---|---|---|---|---|---|
|
1st course of treatment |
2nd course of treatment (n = 22) |
3rd course of treatment (n = 22) |
4th course of treatment (n = 22) |
5th course of treatment (n = 21) |
|
|
Complete remission |
1 (4,5%) |
1 (4,5%) |
2 (9,0%) |
2 (9,0%) |
1 (4,5%) |
|
Partial remission |
10 (45,4%) |
13 (59%) |
14 (63,6%) |
16 (72,7%) |
17 (77,3%) * |
|
Temporary improvement |
7 (31,8%) |
5 (22,7%) |
4 (18,2%) |
3 (13,6%) |
2 (9,0%) * |
|
Lack of effect |
4 (18,2%) |
3 (13,6%) |
2 (9,0%) |
1 (4,5%) |
1 (4,5%) * |
|
Note: p <0.05 - the differences are statistically significant compared with the indicators after the first course of treatment of alpine climatotherapy |
|||||
9 children received pulse therapy with dexamethasone at a dose of 30-40 mg / m2 for 4 days. A positive short-term effect of 3 to 6 months was recorded in 9 of them, from 7 to 12 months in the remaining 3 children. Five children got prescribed with roferon-A, a type of a2-interferon in the following dosage: 500 thousand IU/ day for children under 5 years old and 1 million IU/ day for children from 6 to 14 years old. Children received two courses of roferon A; remission ranged from 3 to 8 months. In the remaining three children, parents refused to prescribe oral steroid hormones, and each time they went to the hospital, they were limited to symptomatic therapy. Remission ranged from 1 to 3 months. Before climbing to the high mountain base Tuya-Ashu, all the children hospitalized in a hematological hospital, where they underwent a full clinical and laboratory examination and, if necessary, they are prescribed with appropriate treatment.
Upon admission to the clinic, manifestations of the hemorrhagic syndrome observed in almost all children. Thus, minimal manifestations of hemorrhagic skin syndrome in the form of single ecchymoses and petechiae, without a "wet" component, were recorded in 15 (46.9%). Severe skin hemorrhagic syndrome with a total manifestation of petechiae, ecchymoses on the skin and mucous membrane, but without bleeding, was observed in 12 (37.5%) of them. Moreover, finally, any manifestations of skin hemorrhagic syndrome and bleeding of any location, often nasal, less often from the oral mucosa were present in 5 (15.6%) children.
The platelet count ranged from 13.4 to 37.5 x109 / L and averaged 21.5 ± 1.71x10 / L. It should note that in 2 children, this indicator was below the critical level (13.4 and 17.1 x 109 / L, respectively). Years of experience, highlands showed first days of stay in the mountains; there is a decrease in the number of platelets, which is redistributive. In this regard, before climbing the mountains, four children with severe hemorrhagic syndrome received a platelets transfusion (two doses once). Besides, two children with platelet counts below the critical level were prescribed pulse therapy with dexamethasone at a dose of 30-40 mg / m2 for 4 days.
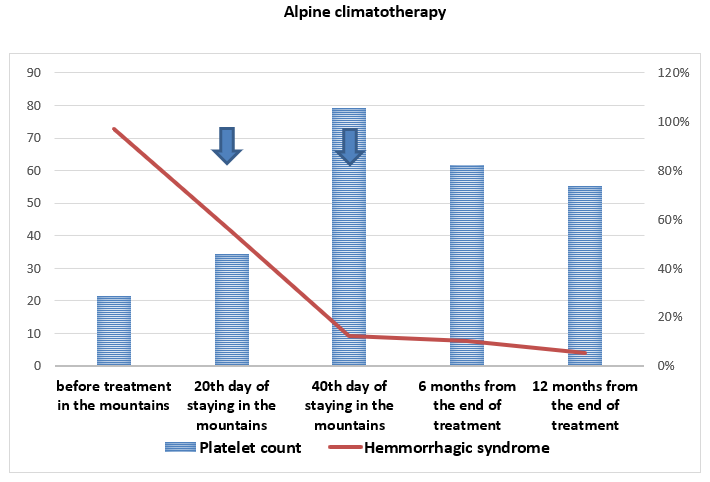
For the safe transition of the adaptation period in the highlands, from the first day in the mountains, strict bed rest was prescribed with a duration of 5-7 days. If, during this period, there was no increase in hemorrhagic syndrome, walks around the hospital were allowed, followed by a gradual climb to the mountains. Starting from the 20th day of stay in the mountains, a noticeable improvement in the condition and an increase in the number of platelets observed (Figure 2). So, while before high-altitude climatotherapy, hemorrhagic syndrome manifestations were present in all patients, on the 20th day in the mountains, they persisted only in 8 children. The optimal changes in the condition of sick children came at the end of their stay in the mountains. By the 40th day of high-altitude climatotherapy, a hemorrhagic syndrome in 28 children had stopped, the remaining 4 retained only minimal manifestations of the hemorrhagic syndrome.
Following the relief of hemorrhagic syndrome, an increase in the number of platelets noted. So, starting from the 20th day of stay in the mountains, the number of platelets is started to grow; their average number is 34,2±1,37 thousand / μl (p <0.05). By the end of the term, that is, on the 40th day of stay in the mountains, the increase in platelet count reached its maximum, averaging 79,3±2,51 thousand / μl (p <0.05).
In the long-term period (6 and 12 months), the level of platelet count decreased to 61,7±3,11 thousand / μl and 55,1±1,73 thousand / μl, respectively. However, the values are also higher than the initial values before treatment. The treatment results evaluated by the following criteria: complete remission (platelet count of more than 100 thousand / μl, hemorrhagic syndrome stopped); partial remission (platelet count less than 100 thousand / μl, hemorrhagic syndrome stopped); temporary improvement (platelet level above a critical value for 6 months) of hematological parameters and lack of effect.
Of the 32 children who received high-altitude climatotherapy once, two achieved complete, and fourteen had partial remission. In eleven children, the improvement of clinical and haematological parameters was temporary, and the absence of effect recorded in five patients. It is clear that, despite the absence of the effect of alpine climatotherapy, the children during the year of observation did not have an apparent exacerbation of the disease and, consequently, hospitalization in a hospital. The results showed that 50% of children with chronic ITP responded positively to a single high-altitude climatotherapy. Since 2015, 22 children have continuously received high altitude climatotherapy. From (Table 1), repeated courses of alpine climatotherapy showed an increase in the number of children with clinical and haematological remission.
As can be seen from (Table 1), complete remission registered in one child, after the third course, a second one joined, but this child was not able to receive a full course of the fifth treatment due to family circumstances. Partial remission after the first course of treatment observed in 10 patients, but after each subsequent treatment, the number of such children increased and reached 17 children. Due to the increase in the number of children with partial remission, there was a decrease in patients with temporary improvement and lack of effect, clearly shown in (Table 1).
Demonstration of the effectiveness of therapy with an alpine climate, the clinical case of a child with complete remission is given below, which has been observed in our country since 2015 with a clinical diagnosis: severe ITP (initially generalized skin-hemorrhagic syndrome, platelet count below 20x109 / l.).
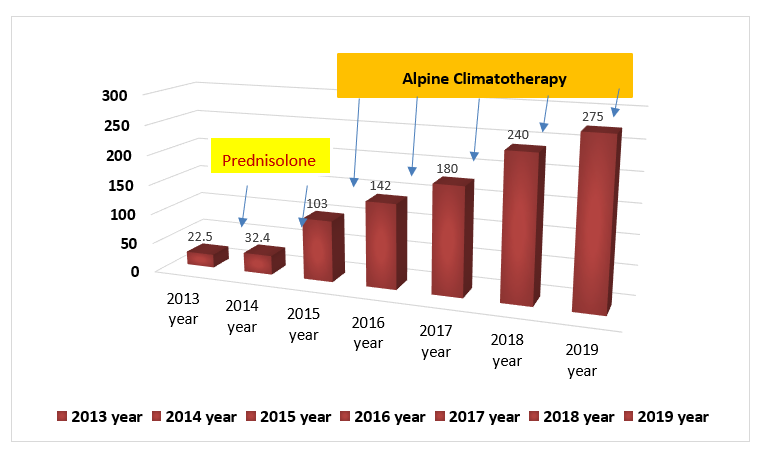
Child SA, 06/01/2010 year of birth, the patient considers herself ill from October 2013, the first time a clinical diagnosis of immune thrombocytopenia (ITP) done by the haematology department of the National Center for Maternal and Child Health of the Kyrgyz Republic. For a year and a half, she received glucocorticoid therapy (prednisone 2 mg per 1 kg of body weight). During the treatment, the skin hemorrhagic syndrome and nosebleeds continually recurred, the platelet count remained at the level of 25-35x109 / l. During this period, the child had 7 hospitalizations in the hospital, and each hospitalization lasted until 15-20 days. Due to the inefficiency of the first line glucocorticoid therapy in July 2015, the patient first referred and taken for a 40-day course of treatment with high-altitude climatotherapy. The child completed the full course of treatment. If before ascending the mountains, the platelet count was 32.4 x 109 / L, then after the course, their number reached 103.0 x 109 / L (Figure 3). Manifestations of the skin-hemorrhagic syndrome stopped entirely.
The achieved remission remained stable throughout the year, with no hospitalization until the next treatment in the mountains. Thus, a child S.A. received a full five-fold course of alpine climatotherapy in total (2015, 2016, 2017, 2018 and 2019). On September 1, 2017, after a three-time stay in the mountains, the child successfully went to the first grade of a secondary school in Bishkek frequently. The dynamic changes of the platelet count after each course of treatment shown in (Figure 3). Today, the child has fully recovered; over the past two years, the platelet count has remained above the minimum average level.
The clinical case in this article shows the high efficiency of the high-altitude climatotherapy as an alternative treatment of immune thrombocytopenia (ITP). The result shows complete clinical and haematological remission and achieved a complete recovery of the child. In the meantime, the child will be under our supervision. The remaining children with immune thrombocytopenia who receive high altitude climatotherapy also responded positively to treatment in the form of partial remission and haematological improvement. The effect of the highlands assumed that the positive effect of the highlands because,
1) Hypoxia contributes to the increased production of thrombopoietin, which stimulates the megakaryocytic bone marrow growth, increases the number of platelets in the peripheral blood and
2) Increase in the production of glucocorticoids in the mountains does not exclude their immunosuppressive effect, given that most thrombocytopenia is autoimmune.
Conclusions
High altitude conditions contribute to the improvement of the clinical signs in children with chronic immune thrombocytopenia (ITP), a significant increase in platelet levels in peripheral blood and the achievement of remission in most of them. The experience of haematological clinic is significant. It allows participating in the optimization of therapeutic approaches in the treatment of immune thrombocytopenia and especially its chronic form, the undertaken studies, in our opinion, can be considered a promising area that requires further evidence and confirmation on a large number of patients.